Implementing an Entrustable Professional Activities (EPA)-based medical curriculum marks a profound transformation in how we approach medical education. It moves the focus away from abstract competency checklists and towards the real-world responsibilities that define day-to-day clinical practice. However, as with any major shift, making this transition effectively requires careful planning and structured execution. Drawing on years of experience supporting teaching hospitals with EPA implementation, here are the three essential steps that any institution should follow when embedding EPAs into their medical curriculum.
Step 1: Defining the EPA framework for your medical program
An EPA is not just any task a trainee might perform; it must meet specific criteria to ensure it fits within an entrustment-based model. Each EPA should be essential to professional practice, involve a patient safety risk that necessitates an entrustment decision, be observable and assessable in a clinical setting, and result in a tangible outcome. For instance, managing a patient with pneumonia or obtaining informed consent for surgery are strong examples of EPAs. In contrast, activities like attending lectures or demonstrating theoretical knowledge, while valuable, don’t meet the threshold for EPAs and should be addressed differently.
Institutions must also strike a balance in the number of EPAs included. Too few risks missing critical training elements, while too many can overburden both learners and faculty, diluting the clarity and focus of the curriculum. Based on international experience, a range of ten to twenty EPAs per specialty tends to offer the right mix of comprehensiveness and manageability. Once identified, EPAs should be categorized into two groups: core EPAs, which all trainees must achieve regardless of their individual path, and specialty-specific EPAs, which relate to particular rotations or disciplines.
Not every activity will qualify as an EPA, but that doesn’t mean these tasks should be discarded. They often underpin EPA performance and should be mapped to supporting competencies or assessed using alternative methods such as written exams, OSCEs, or feedback tools. This ensures that your program remains comprehensive, with every important aspect of training accounted for.

Step 2: Redesigning the curriculum to integrate the defined EPAs
This requires careful mapping of where each EPA fits into the training timeline, ensuring students are introduced to, practice, and ultimately master each EPA in a logical progression. Core EPAs should be spread across general phases of the curriculum, ensuring every learner builds a solid foundation. Specialty-specific EPAs, in contrast, can be introduced later when students have chosen their particular clinical path.
This restructuring is more than just a logistical exercise, it demands a shift in teaching methods as well. To integrate EPAs into day-to-day learning, institutions must adopt a supervision progression model. This model follows five levels of supervision, starting from simple observation and culminating in independent execution and even supervising others. At each level, trainees develop not only their skills but also the trust of their trainers. This scaffolding of responsibility ensures a safe, structured path towards independence.
Step 3: Align stakeholders
A successful transition to EPA-based education hinges on the commitment of everyone involved, from faculty to trainees. For trainers, this shift means adapting their approach to assessment, feedback, and decision-making. They must learn to observe performance in real clinical contexts, provide timely and actionable feedback, and make entrustment decisions that reflect a learner’s readiness for independence. This requires specific training in the use of assessment tools, rubrics, and structured feedback models.
Consistency in assessment is another common challenge. Different educators may interpret entrustment standards in different ways, leading to variability in learner outcomes. To mitigate this, institutions should implement regular calibration sessions, clear assessment rubrics, and faculty development programs that align expectations and promote shared standards.
Equally important is the engagement of learners themselves. They must understand how EPAs function, how they will be assessed, and how to take ownership of their learning journey. Transparency around learning goals, the use of digital portfolios to track progress, and the promotion of self-assessment and reflection all contribute to a more empowered and proactive learner.
Final thoughts
The shift to EPA-based education is more than a curriculum update, it’s a cultural transformation. It redefines how we think about medical training, focusing on trust, performance, and real-world readiness. While the journey may seem daunting, a structured, step-by-step approach, defining the EPA framework, integrating it into the curriculum, and aligning all stakeholders, makes this transformation not only manageable but deeply rewarding. By doing so, institutions create a learning environment that better prepares future healthcare professionals for the complex, high-stakes responsibilities they will face in practice.
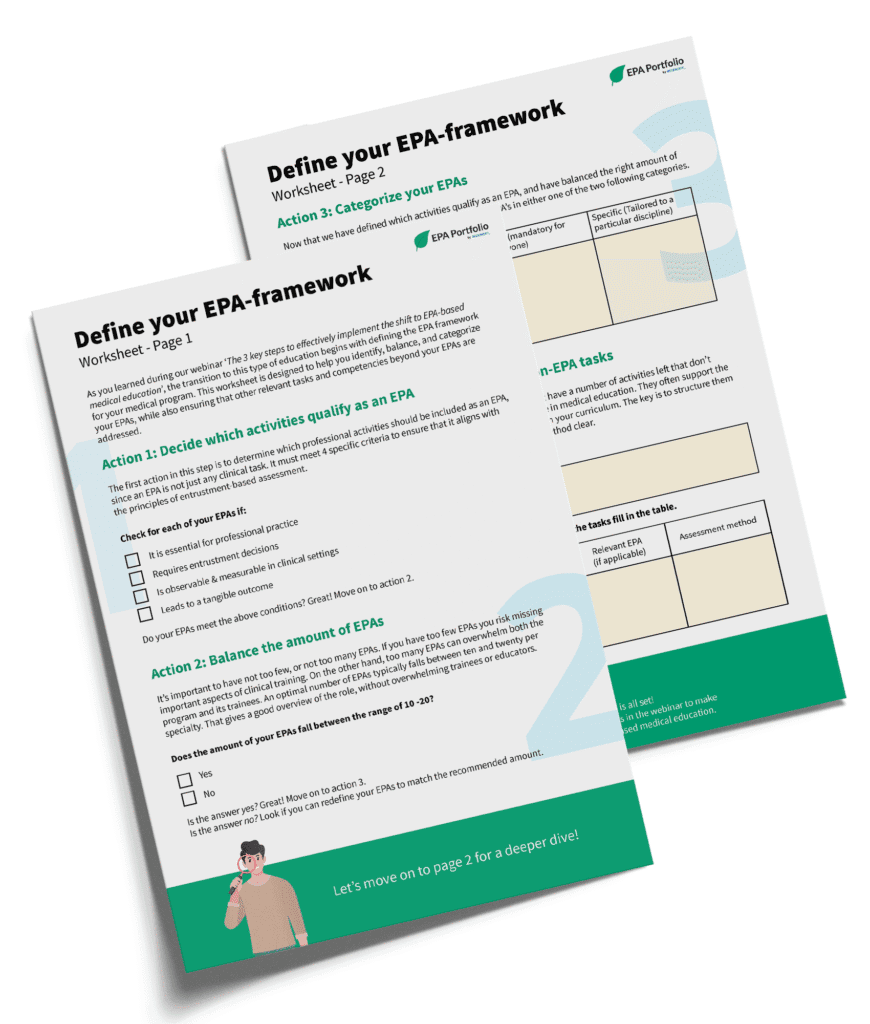
Download our interactive worksheet
We’ve created a free, interactive worksheet to help you take the first step in implementing an EPA-based medical curriculum: defining the EPA framework for your program. This worksheet supports you in identifying and organizing your EPAs, while also ensuring that other essential competencies, beyond the EPAs, are addressed. Fill out the form below, and we will send you the worksheet right away by email!